EAACI Newsletter, October 2004 – Issue 3
Report from Amsterdam - Report from Plenary Session (PS3)
Allergic inflammation
The following article presents some of the latest thinking on allergic inflammation, including hypotheses on a new target for treatment, siglecs and a protein that may be important in asthma.
The allergic inflammation process has different stages. First comes the allergen presentation. The afferent phase is characterised by allergen uptake, e.g. by dendritic cells and migration to the lymph nodes.
Communication pathways of epithelial cells consist of pattern recognition receptors (Toll-like receptors) and the effector
mediators, such as defensins, cytokines and chemokines. The efferent phase commences with the production of TSLP
(thymic stromal lymphopoitin), produced in tonsillar crypt epithelial cells. Dendritic cells survive and start their maturation
under the influence of TSLP. In atopic dermatitis, TSLP is overexpressed triggering the inflammation by recruitment and
priming of T-cells.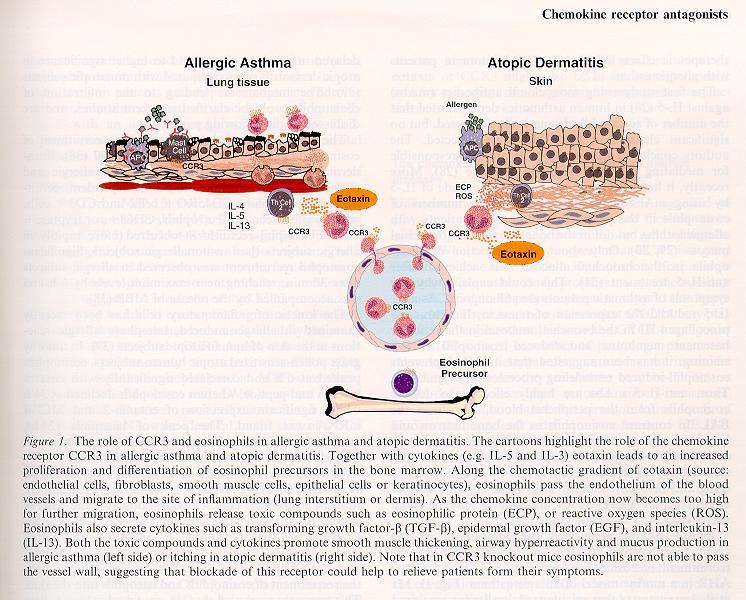
The next step is modulated by the production of chemokines, such as IL-4, -5 and -13. They attract leucocytes by chemotaxis. This is achieved first by making the vessel wall express adhesion molecules so that the cells can attach at the site of inflammation, and later, by extravasation and migration in the direction of the highest concentration.
Dendritic cells (DCs) migrate to draining lymph nodes. In this way, memory T-cells can teach the adaptive immune system. DCs are regulators of the allergic immune response. There are several subtypes found in humans and mice. They include myeloid DCs and plasmacytoid DCs.
New target for therapy?
The following hypothesis was recently presented: antigen presentation by myeloid DCs leads to sensitisation while antigen presentation by plasmacytoid DCs leads to tolerance. The number of CDla+ DC is increased in the airways of allergic rhinitis patients and can be further increased by allergen challenge. A decrease can be obtained through nasal steroids. As a conclusion, one can state that m-DCs induce sensitisation if properly activated while p-DCs suppress sensitisation to inhaled harmless antigen in baseline conditions. However, it remains an open question whether DCs can be the next target for therapy.
Some recent publications on the advances in allergic inflammation have focused on siglecs. These are a subset of the
immunoglobulin gene superfamily, possessing a domain with sialic acid binding activity. They have a regulatory function on
eosinophil, mast cells and basophils. Siglec-8 is found in the lungs, spleen and the peripheral blood cells. From the point of
view of genetics, many siglecs are located in a genetic region closely linked to asthma on chromosome 18.
The role of siglecs
A survey of Siglec 8 surface levels shows that the blood cell expression is equal to the BAL cell expression and that allergic eosinophils and non-allergic eosinophils are equal. Furthermore, the levels are unaffected by cytokines, chemokines or other mediators. The hypothesis is therefore postulated that siglec crosslinking could induce eosinophil death. This phenomenon was detectable within four hours. This apoptosis could not be prevented by survival-promoting cytokines. The siglec 8 induced eosinophil apoptosis can be inhibited by the Pan Caspase inhibitor Z-VAD-FMK. Siglec 8 ligation induces Caspase activity. Caspase-dependent apoptosis in eosinophils and crosslinking of Siglec -3, -5 or -8 inhibits IgE dependent basophil histamine release.
Proteins implicated in remodelling
Matrix Metallo Proteinase (MMPS) and Tissue Inhibiting Proteinase (TIMPS) are proteins that are responsible for the remodelling of the extracellular matrix. For example in asthma, the balance between TIMPs and MMPs in the local inflammation strongly determines the outcome of the disease.
MMPs can have very disruptive effects on tissue. The remodelling effects that they cause are fibrosis, smooth muscle hypertrophy, vessel formation, mucus gland hypertrophy and ECM deposition. The family of MMPs consists mainly of gelatinases (MMP2 and9), collagenases (1, 8, 13 and 18), stromilysins (3, 10, and 11), membrane type MMPs (14, 15, 16, 17 and 24) and matrilysins (7 and 26). The regulation of MMPs is done by gene- or pro enzyme activation, or by inhibitor inactivation. The aspecific inactivators and specific inactivators are callled TIMPS. Except for MMP 7 and 28, which do not have a hemopexin domain, the domain structure of MMP consists of a signal peptide, a propeptide, a catalytic domain and a hemopexin domain.
The catalytic domain is the part containing a zinc atom, from which arises the "metallo" in Matric Metallo Proteinase. This is also the enzymatic active part of the protein. Because of the colocalisation of MMP 9 and 3 with inflammatory cells, they probably play an important role in asthma.
Studies show a significant increased MMP 9 and TIMP 1 activity in severe asthma. The gelatinolytic activity can be measured by zymography and immune assay on BAL fluid of asthmatics. It is shown to be much higher when disease is present. MMP 9 levels increased the day of an asthmatic attack and drop again slowly over a period of 28 days. After allergic provocation MMP 9 levels raised slower than TIMP 1 levels. Neutrophils are a primary source of MMP 9 in the airway lumen. The effect of treatment was also measured, showing a drop of collagen III deposition and submucosal MMP-9 expression after inhaled glucocorticosteroid therapy.
The role that MMPs play in asthma relates to the degrading of ECM proteins, the promotion of cell trafficking, the release of peptides and chemokines from ECM, the activation of growth factors and the release of cell surface receptor molecules. Their contribution to asthma depends on the activation and the inactivation of their inhibitors. The balance is delicate between MMPs, which are there for degradation, inflammation and injury, and MMPs, which promote fibrosis, growth and repair. Jeroen Clemen
t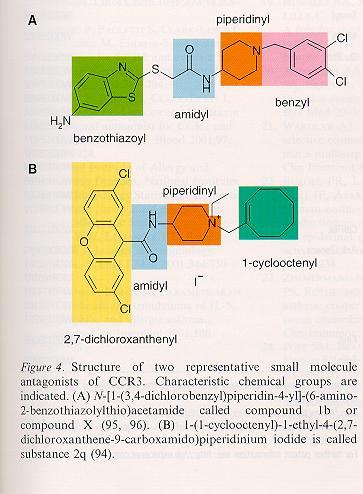
Report from the JMA Symposium
Uncovering Neuro-immunological Influences in Allergy
and Clinical Immunology
The influence of brain activity on the soma is a theme that has fascinated humans from thedawn of human civilisation.
In the modern age, thinkers since Descartes and Freud and right up to contemporary investigators, such as Damasio and Goleman, have put forward their ideas on various ways to link the brain with the body. Nowadays, detailed scientific evaluations correlating brain function, such as working memory and decision making, with bodily change (performance) can be made with the aid of modern methods. e.g., PET and FMRI.
Psychoneuroimmunology is a new interdisciplinary field concerned with investigating the effects of psychological factors on the nervous and immune systems and their interactions. There is increasing evidence from both animal and human studies that stress results in cell activation and the releases of certain compounds. More specifically, stress creates concomitant activation of cells from the nervous, endocrine and immune systems. It also leads to the release of diverse biologically active compounds, including glucocorticoids, catecholamines, neuropeptides and cytokines. Dr R.A. Joachim demonstrated that exogenously applied stress dramatically enhances airway reactivity and airway inflammation via the neurokinin-1 receptor, which is the main receptor for the tachykinin substance P.
From daily practice, we know that many asthma patients claim to have experienced stress-induced asthma attacks. Several studies confirmed that prolonged stress is associated with increased eosinophilic airway inflammation, negative mood and other miscellaneous symptoms. When lung function remains reduced, stress may also cause relatively mild breathlessness.Empirical support for acute stress effects is less robust. Dr. S. Rietveld measured the acute effects of positive and negative stress on parameters of asthma via exposure to roller coasters, itching powder, impossible computer games and public intelligence tasks.
Overall, only a minority of patients react with a fall in lung function, which does not correlate with respiratory changes, eosinophil count, or breathlessness. The expression of breathlessness is dominated both by patients positive or negative feelings and by the presence or absence of a context that patients have learned to associate with asthma.
Irrespective of lung function, chronic asthma patients are likely to perceive breathlessness during negative stress in an asthma context. They are unlikely to perceive breathlessness during positive stress in a non-asthma context.
Complementary medicine
In western societies, patients with chronic disease, such as those suffering from allergic disease, are increasingly likely to seek help from complementary and alternative medicine (CAM). A wealth of unsystematic reports exists showing that CAM may be beneficial for the treatment of asthma. However, hard evidence from clinical trials is rarely available in the medical literature.
Moreover, when the small number of existing clinical trials is examined with the help of rigorous meta-analysis, the effects rarely reach significance.
We know that many
asthma patients claim
to have experienced
stress-induced asthma
attacks.
In the face of a paucity of hard facts, why does CAM attract an ever-growing body of followers? Have the effects of CAM treatments been inappropriately researched? Are CAM treatments too diverse to be measured through the methods of conventional medicine? Do we need to unravel the myths about CAM in order to judiciously advise on CAM treatments? If not, what are the alternatives? Philippe Gevaert
EAACI Newsletter
Report from Main Sympo (MS4)
Aero biology and Pollution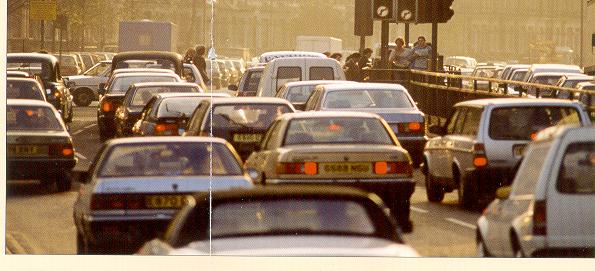
The significance of aerobiology for allergological research was the first point that Frits Spieksma stressed in the introduction of this Main Symposium.
He explained that allergens do not occur airborne as individual molecules, but they are present in both the outdoor and indoor air carried by small respirable particles, mostly of sizes under 50 micrometre.
The study of these allergen carrying particles, such as fungal spores, pollen grains, mite faecal pellets, animal skin scales, etc., is a major field of interest in the science of aerobiology. These studies include the launching, the transportation, and the deposition of the particles. But in a wider definition of aerobiology also the occurrence of the particle sources or producers (like anemophilous plants, mites, etc), as well as the mechanisms of deposition in the respiratory tract and the effects in allergic people (like rhinitis and bronchial asthma) are taken into consideration. It is clear that for a complete understanding of the incidence and epidemiology of allergic symptoms solid knowledge of aerobiological phenomena and processes is essential, concluded Frits Spieksma.New allergenic plants and pollen forecasting is a raising problem in Europe explained Pro£ Giuseppe Frenguelli. He pointed at ragweed pollen as an important and increasing allergen in central Europe and called the attention to those new species planted that have increased pollen sensitisation and allergic disease. We should care about which plants are chosen to be in our towns and/or gardens. The new plants should not have aggressive pollination to avoid the increase of sensitisations and allergies. The different methods of forecasting involve monitoring pollination and the urban climate effect (building density, diesel particles, etc) and increasing the allergenicity of urban pollen must not be forgotten. Nevertheless, in the words of Prof. Frenguelli, the environmental factors causing the increase in allergic diseases remain unknown.
In this respect, the second speaker, Prof. Isabella Annesi-Maesano pointed to the differences between pollen exposure, pollen sensitisation and pollen allergy, depending on environmental and other individual factors. Among these factors diet, number of infections, stress, neonatal factors and other unknown incidences were mentioned. We cannot consider hay fever as only a disease due to pollen hypersensitivity. Asthma and cutaneous diseases such as eczema should be also considered from epidemiological point of view. Anyway, it is very difficult from a political point of view to predict the impact of pollenosis on public health.
lndoor allergens
There is a strong correlation between house dust mites and cockroach exposure and asthma stressed Prof. Platts-Mills. Referring to cat allergens, he explained that no agreement exists among different authors in different countries. In the opinion of those working in Northern Europe, cat exposure has a protective effect for the development of bronchial asthma while those from New Zealand think that exposure to house dust mites and cat allergens can potentiate each other. In any case there is not a convincing explanation for either theory. The experience with mould allergens is not sufficient and more work is still needed in this field.
Finally, the Chairman of the EAACI Interest Group "Aerobiology and Pollution", Pro£ Gennaro D'Amato, updated what is known about the impact of urban air pollution on respiratory allergy. Both the prevalence and severity of respiratory allergic diseases, such as bronchial asthma, have increased in recent years. Among the factors implicated in this "epidemic" are indoor and outdoor air-borne pollutants.
Outdoor allergens
Urbanisation, with its high levels of vehicle emissions and westernised lifestyle, parallele the increase in respiratory allergy in most industrialised countries, and people who live in urban areas tend to be more affected by the disease than those of rural areas. In atopic subjects, exposure to air pollution increases airway responsiveness to aeroallergens. Pollen is a good model with which to study the interrelationship between air pollution and respiratory allergic diseases. Biological aerosols carrying antigenic proteins such as pollen grains or plant-derived paucimicronic components can produce allergic symptoms. By adhering to the surface of these airborne allergenic agents, air pollutants could modify their antigenic properties. Several factors influence this interaction, i.e., type of air pollutant, plant species, nutrient balance, climatic factors, degree of airway sensitisation and hyperresponsiveness of exposed subjects.
However, the airway mucosal damage and the impaired mucociliary clearance induced by air pollution may facilitate the penetration and the access of inhaled allergens to the cells of the immune system, and so promote airway sensitisation. As a consequence, an enhanced IgE mediated response to aeroallergens and enhanced airway inflammation favoured by air pollution could account for the increasing prevalence of allergic respiratory diseases in urban areas.
All these talks contributed to a wider view of what actually is known about the interaction between pollinosis and environmental factors. As shown in aerobiological and allergological studies, the pollen map of Europe is changing as a result of cultural factors and the increase of international travel explained Marta Orta, Secretary of the EAACI Interest Group "Aerobiology and Pollution". The dissection of the relative contribution of environmental and genetic factors will provide a deeper understanding of the pathophysiology of allergic disease. Ignacio Ansotegui
To these matters look also at www.rki-i.com , R.Kiehl, Publications and Materials (book-chapters and
powerpoint-presentations, free download as pdf- or html-files)
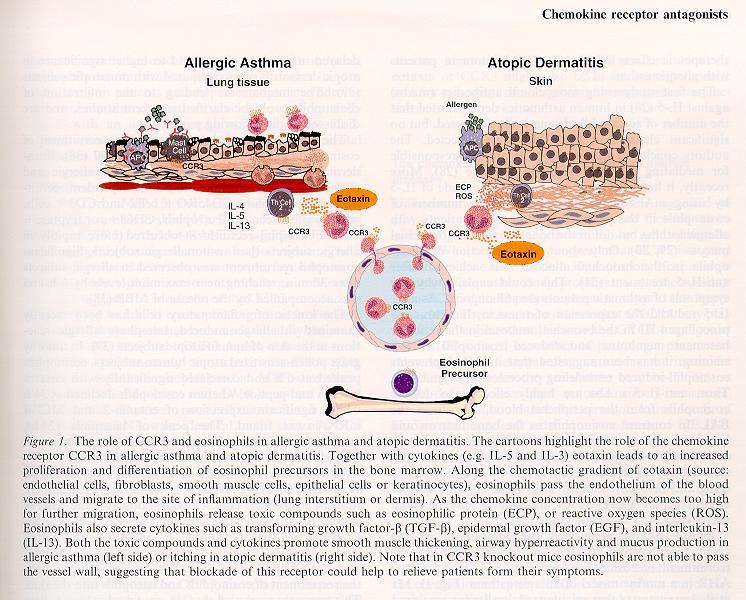
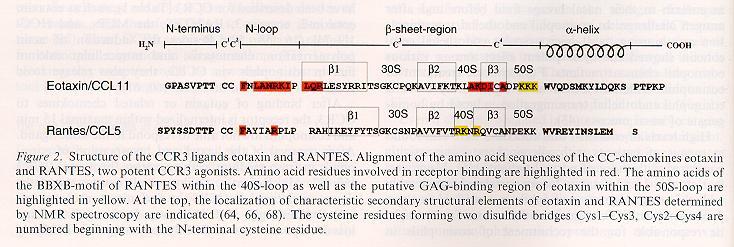
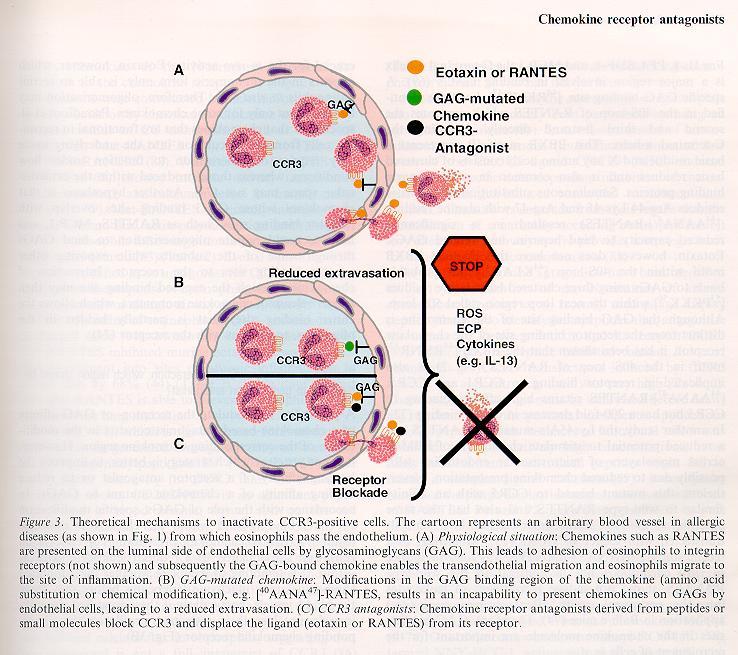
Figure 1 to 4 out of the review article: Chemokine receptor antagonists: a novel therapeutic approach in allegic disease. Allergy 2004: 59:1243-1258 (Printed in UK)